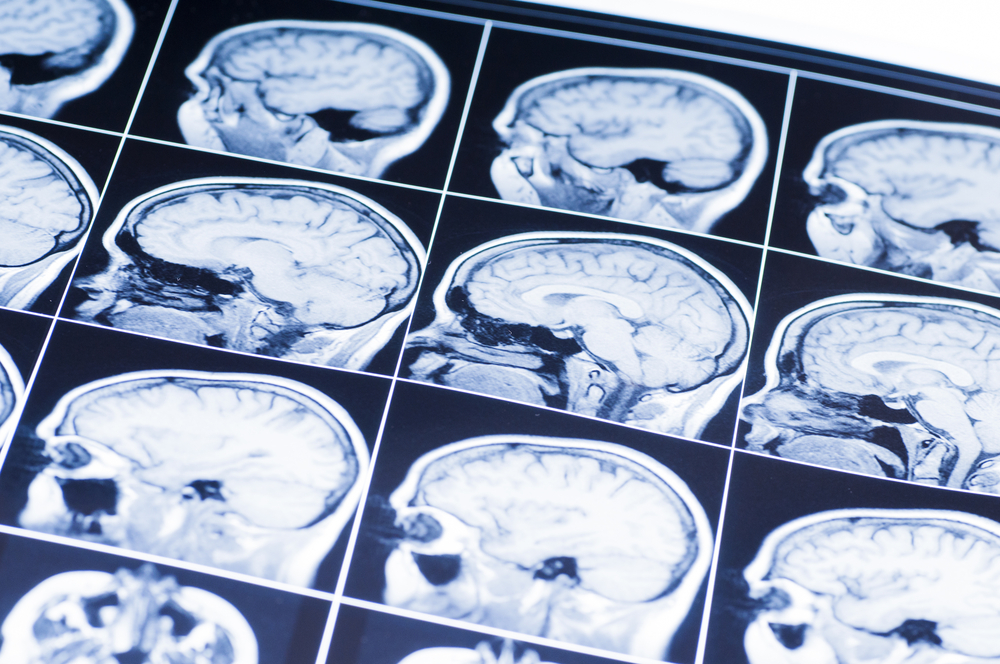
Achieving pristine MRI scan quality requires patients to stay perfectly still for extended sequences amid loud, jostling magnetic environments within units.
But for anxious, uncomfortable individuals inside cramped open MRI machine image, remaining motionless grows challenging even through shorter exam durations.
Subtle motions during Gadolinium contrast administration or standard T1/T2 protocols easily manifest as visual blurring or ghosting on images.
Yet proper positioning fundamentals using immobilization tools, sequence education, and comfort aids counteract restless tendencies minimizing motion distortions.
Here are best practices for patient staging and preparation ensuring immaculate open MRI imaging beyond just hitting start:
Orient Patient Posture Purposefully
Align patient positioning early on first entering the MRI room based on targeted anatomy and protocol goals. This sets a solid stillness foundation before scanning begins.
For examinations like lumbar spine imaging, ensure the patient lies with their lower back evenly contacting the table surface if flat sequences are needed.
But tilt slightly if capture oblique’s. Always centralize regions of interest within center open bores.
Strategically place pads, and wedges and adjust table heights reducing uneven weight distribution or tissue strain which commonly provokes fidgeting as sequences progress when discomfort emerges.
Have patients adjust arms, grasp handles allowing muscles to relax during acquisitions.
Just ensure limbs fully cleared of imaging regions. Getting posture precision before sessions prevents preventable motion issues downline.
Employ Immobilizing Devices and Supports
Where exam durations run extensive (30+ minutes) or patients express movement difficulties beforehand, utilize selective immobilizing supports redistributing weight, and stabilizing extremities.
Positionable foam pads, vac-lok cushions, strapped pillows, or contoured mattresses all encourage better conformation anchoring the body in place as the scan progresses.
Inflatable HeadMotion pads limit subtle head rotations during neuro examinations. Custom thermoplastic masks also generated from molds of faces or extremities help in certain cases.
Blankets, towels, and other fabric items should be avoided though unless vetted as MRI-safe materials gave projectile risks interfering with magnetic lines.
Communicate Sequence Instructions Clearly
Unprepared patients startle moving when deafening pulse sequences suddenly start alongside vigorous table vibrations.
Quelling reactions rely on deliberately educating what loud noises and sensations manifest during portions of upcoming scan sessions:
“You’ll hear pulsing tones when imaging runs just like hammer blows. The cushion may shake a bit but everything is normal.
I’ll check on you between stronger sequences but remain still as able until staff returns to the room.”
This positions proper expectations minimizing reactions scrambling when unaware sequences commence.
Show patients scan initiation triggers like squeeze balls so they recognize when active periods start enabling voluntary stiffening.
Perform Comfort Checks Between Sequences
For exams exceeding 20 minutes, periodically enter scanning rooms between administered sequences to gauge patient pain levels and reconfirm immobilized positioning stays intact.
Scan delays from motion often trace back to leg cramps, neck strains, or arm numbness building over time left unaddressed.
So proactively inspect comfort and technique, adjusting supports preventing uncontrolled sudden movements overcoming pain thresholds.
Quick confirmations also remind patients when the next sequence commences so they ready themselves mentally avoiding startled reactions. Remaining vigilance until exams finish ensures motion reduction follow-through.
With deliberate posture crafting, supportive gear utilization and patient guidance – technologists minimize open MRI motion likelihoods despite the inherent environ challenges.
Following fundamental best practices optimizes imaging accuracy when precision matters most diagnostically. So take time initially positioning for success.

